Background:
Despite the widespread use of platinum-based combination chemotherapy, particularly when complemented with taxanes, for the treatment of gynecologic malignancies, its administration often results in myelosuppression. This effect can be potentiated across cumulative chemotherapy cycles, thereby inducing a more persistent condition known as cancer therapy-induced thrombocytopenia (CTIT). Traditionally, preferred treatments for CTIT entail platelet transfusion or the use of recombinant human thrombopoietin (rhTPO), or recombinant human interleukin-11 (rhIL-11). However, the efficacy of platelet transfusion tends to decrease with repetitive administration, and it carries inherent risks of infectious diseases. Additionally, rhIL-11 may induce severe hypersensitivity reactions, necessitating permanent discontinuation of the drug. Emerging as an appealing alternative, thrombopoietin-receptor agonists (TPO-RAs) present a promising approach for CTIT treatment. Among these, hetrombopag, an orally administered small-molecule TPO-RA, has demonstrated notable platelet-boosting effects and a favorable safety profile not only in patients with immune thrombocytopenia and severe aplastic anemia but also in those suffering from persistent CTIT. This study aims to appraise the real-world effectiveness and safety of hetrombopag, administered either alone or in conjunction with other platelet-boosting agents, for the management of CTIT in patients diagnosed with gynecologic malignancies.
Methods:
In this retrospective study conducted from January 2022 to June 2023, we examined the role of hetrombopag in treating CTIT among patients with gynecologic malignancies. The patients, aged 18 years and above, had experienced thrombocytopenia (platelet counts<100×10 9/L) following platinum-based chemotherapy or other antitumor treatments and subsequently received hetrombopag either as monotherapy or in combination with other platelet-boosting agents, such as rhTPO or rhIL-11. The primary outcome was platelet response within 14 days, denoted by a recovery in platelet counts to ≥100×10 9/L or an increase of ≥50×10 9/L or at least double from the baseline.
Results:
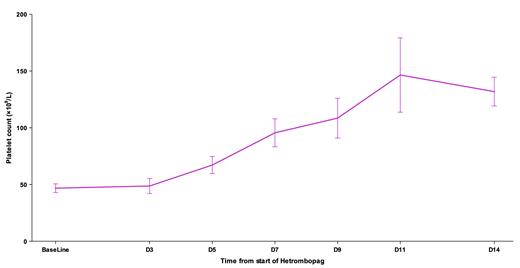
This study comprised 38 patients, with 55.3% diagnosed with ovarian cancer, 36.8% with cervical cancer, 5.3% with endometrial cancer, and 2.6% with other types. The median age was 58 years, with the majority (73.7%) at clinical stages III/IV. As for the antitumor regimens, 89.5% incorporated platinum, 68.4% included taxanes, 26.3% used antiangiogenic agents, and 15.8% employed PD-1 inhibitors. Among the patients, 15.8% received hetrombopag 2.5 mg/day monotherapy, while the remainder received hetrombopag in combination with rhTPO or rhIL-11. Baseline platelet counts prior to hetrombopag therapy averaged 46.5±24.9×10 9/L. Encouragingly, the 14-day platelet response rate was 71.1%, with a median time to response of 10 days (95% confidence interval, 5-14). Following treatment with hetrombopag, patients exhibited a gradual increase in platelet levels, recording mean platelet counts of 48.7, 67.1, 95.5, 108.5, 146.5, and 131.9×10 9/L on days 3, 5, 7, 9, 11, and 14 respectively. Importantly, hetrombopag was well-tolerated, with no treatment-related adverse events observed during the treatment course.
Conclusion:
In conclusion, our findings suggest hetrombopag, either alone or in combination with other therapies, displays preliminary effectiveness and safety in treating CTIT. Given its convenient oral administration and promising platelet-boosting effects observed in this study, prospective investigations of hetrombopag monotherapy for CTIT in gynecologic malignancies are warranted.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal